Death is an inevitable part of life, and exploring the least painful way to die has become an increasingly important topic in modern discussions about end-of-life care. As medical advancements allow people to live longer, the focus has shifted toward ensuring that the final stages of life are as comfortable and dignified as possible. Whether due to terminal illness, aging, or other factors, understanding the options available can empower individuals and their loved ones to make informed decisions.
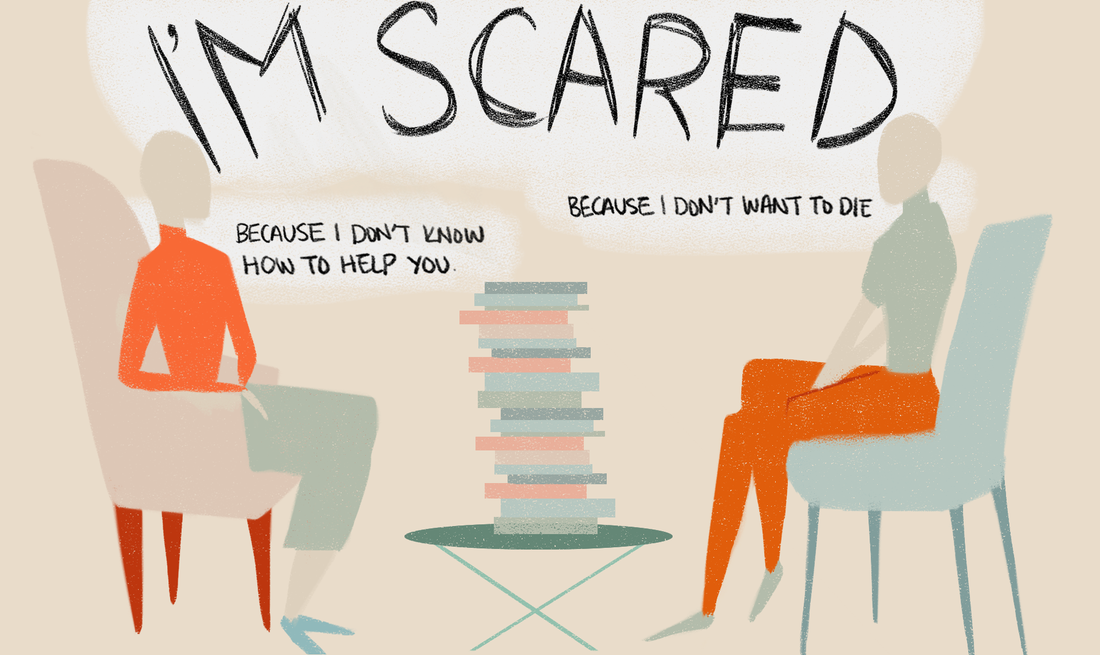
End-of-life choices involve not only medical considerations but also ethical, emotional, and spiritual dimensions. This article delves into the least painful ways to die, examining various methods and approaches that prioritize comfort and peace. By exploring the science behind pain management, palliative care, and compassionate practices, we aim to provide clarity and guidance for those navigating this sensitive subject.
It is crucial to approach this topic with sensitivity and respect for individual preferences and beliefs. The goal is to minimize suffering and ensure that the final moments of life are met with dignity and care. Through this article, we hope to shed light on the least painful way to die while respecting the complexities of human experiences.
Read also:Michael Clarke Duncan The Iconic Height And Weight That Defined A Legend
Table of Contents
- Biological Aspects of Death
- The Role of Palliative Care
- Methods Considered Least Painful
- Ethical Considerations in End-of-Life Decisions
- A Medical Perspective on Pain Management
- The Spiritual Dimension of Dying
- Legal Issues Surrounding End-of-Life Choices
- Modern Pain Relief Techniques
- Compassionate Care in Practice
- Conclusion and Next Steps
Biological Aspects of Death
Death is a natural biological process that every living organism experiences. Understanding the biological aspects of death provides insight into what makes certain methods less painful. The body undergoes several stages during the dying process, including the cessation of organ function, brain activity, and eventually, cellular death. The least painful way to die often involves minimizing the body's distress during these transitions.
Key biological factors to consider:
- Shutting down of vital organs
- Decrease in oxygen supply to the brain
- Release of natural pain-relieving chemicals
Research from reputable sources such as the National Center for Biotechnology Information (NCBI) highlights the importance of managing pain during these stages. By understanding the biological processes involved, healthcare providers can offer more effective end-of-life care.
What Happens to the Body?
During the dying process, the body experiences a series of changes that can influence the level of pain. For instance, the heart rate slows down, breathing becomes irregular, and consciousness may fade. These changes are natural and can be managed with appropriate medical interventions.
The Role of Palliative Care
Palliative care plays a crucial role in ensuring the least painful way to die. It focuses on improving the quality of life for patients and their families facing serious illnesses. Unlike curative treatments, palliative care addresses symptoms, pain, and emotional distress, providing comprehensive support during the end-of-life journey.
Benefits of palliative care:
Read also:Frank Gingerich A Comprehensive Exploration Of His Life Achievements And Legacy
- Reduction of physical pain
- Emotional and psychological support
- Coordination of care among healthcare providers
According to the World Health Organization (WHO), palliative care should be integrated into healthcare systems worldwide. This approach ensures that patients receive the care they need, regardless of their location or financial situation.
How Does Palliative Care Work?
Palliative care teams consist of doctors, nurses, social workers, and other specialists who collaborate to address the unique needs of each patient. They work closely with families to create personalized care plans that prioritize comfort and dignity.
Methods Considered Least Painful
Various methods are considered among the least painful ways to die, depending on individual circumstances and preferences. These methods often involve medical supervision and aim to reduce suffering as much as possible. Understanding the options available can help individuals and their families make informed decisions.
Common methods:
- Sedation therapy
- Medically assisted dying
- Natural death with pain management
Each method has its advantages and considerations, and it is essential to discuss them thoroughly with healthcare professionals. For instance, sedation therapy involves administering medications to induce a state of unconsciousness, ensuring the patient remains comfortable during the dying process.
Medically Assisted Dying
Medically assisted dying, also known as physician-assisted suicide, is a controversial yet effective method in certain jurisdictions. It involves a physician prescribing medication that the patient can self-administer to end their life peacefully. While not legal in all countries, it is an option worth exploring for those facing unbearable suffering.
Ethical Considerations in End-of-Life Decisions
The least painful way to die is not only a medical issue but also an ethical one. End-of-life decisions involve complex moral dilemmas that require careful consideration. Ethical frameworks such as autonomy, beneficence, non-maleficence, and justice guide healthcare providers and families in making these choices.
Key ethical principles:
- Respecting patient autonomy
- Promoting well-being and minimizing harm
- Ensuring fairness and equality in care
Organizations like the Presidential Commission for the Study of Bioethical Issues provide valuable insights into the ethical dimensions of end-of-life care. Their guidelines emphasize the importance of informed consent and compassionate decision-making.
Respecting Patient Autonomy
Respecting patient autonomy means allowing individuals to make their own decisions about their care, including the choice of the least painful way to die. Advance directives and living wills are legal documents that enable patients to communicate their preferences in advance, ensuring their wishes are honored even if they become incapacitated.
A Medical Perspective on Pain Management
From a medical perspective, managing pain is critical in ensuring the least painful way to die. Pain management techniques have advanced significantly in recent years, offering a range of options to address different types of pain. Healthcare providers use a combination of medications, therapies, and interventions to alleviate suffering and improve comfort.
Modern pain management strategies:
- Opioids and other analgesics
- Nerve blocks and spinal injections
- Alternative therapies such as acupuncture
A study published in the Journal of the American Medical Association (JAMA) highlights the effectiveness of multimodal pain management approaches. By combining different techniques, healthcare providers can achieve better results and minimize side effects.
Challenges in Pain Management
Despite advancements, pain management still faces challenges, such as opioid addiction and resistance to certain medications. Healthcare providers must balance the need for effective pain relief with the risks associated with certain treatments. Ongoing research and education are essential to overcoming these challenges.
The Spiritual Dimension of Dying
The least painful way to die also involves addressing the spiritual needs of individuals. For many, spirituality plays a significant role in how they approach death and dying. Providing spiritual support can enhance the overall quality of care and promote peace and acceptance during the final stages of life.
Ways to support spiritual well-being:
- Facilitating access to religious or spiritual leaders
- Encouraging reflection and meaningful conversations
- Respecting cultural and religious practices
Chaplains and spiritual counselors often work alongside medical teams to address the spiritual dimensions of care. Their role is to provide comfort, guidance, and support to patients and their families.
Addressing Spiritual Needs
Addressing spiritual needs involves more than just religious practices. It encompasses a broader sense of meaning, purpose, and connection. By fostering an environment of openness and empathy, healthcare providers can help individuals find peace and closure during their final days.
Legal Issues Surrounding End-of-Life Choices
Legal considerations are an integral part of exploring the least painful way to die. Laws and regulations vary significantly across countries and regions, affecting the options available to individuals. Understanding the legal landscape is crucial for making informed decisions and ensuring that one's wishes are respected.
Key legal aspects:
- Advance directives and living wills
- Medically assisted dying laws
- Guardianship and power of attorney
Resources such as the National Institute on Aging (NIA) provide comprehensive information on legal issues related to end-of-life care. Their guides help individuals navigate the complexities of the legal system and ensure their rights are protected.
Advance Directives
Advance directives are legal documents that outline an individual's preferences for medical care in the event they become unable to communicate their wishes. These documents empower individuals to have a say in their care, even when they are no longer able to express their desires directly.
Modern Pain Relief Techniques
Modern pain relief techniques offer innovative solutions for ensuring the least painful way to die. Advances in technology and medicine have expanded the options available, providing more effective and personalized care. From cutting-edge medications to non-invasive therapies, these techniques aim to enhance comfort and dignity during the dying process.
Innovative pain relief techniques:
- Transcutaneous electrical nerve stimulation (TENS)
- Virtual reality therapy
- Targeted drug delivery systems
Research published in the Nature journal showcases the potential of these techniques in transforming end-of-life care. By staying informed about the latest advancements, healthcare providers can offer the best possible care to their patients.
Targeted Drug Delivery Systems
Targeted drug delivery systems represent a breakthrough in pain management, allowing medications to be administered directly to the affected areas. This approach minimizes side effects and maximizes efficacy, ensuring that patients receive the relief they need.
Compassionate Care in Practice
Compassionate care is at the heart of ensuring the least painful way to die. It involves treating patients with kindness, empathy, and respect, recognizing their humanity and dignity. By fostering a culture of compassion, healthcare providers can create an environment that promotes healing and comfort, even in the face of death.
Elements of compassionate care:
- Active listening and communication
- Cultural sensitivity and inclusivity
- Ongoing support for families and caregivers
Organizations such as the Hospice Foundation of America advocate for compassionate care in end-of-life situations. Their programs and resources emphasize the importance of empathy and understanding in providing quality care.
Support for Families and Caregivers
Compassionate care extends beyond the patient to include families and caregivers who are often deeply affected by the dying process. Providing them with the support they need can help them cope with their loss and find closure.
Conclusion and Next Steps
Exploring the least painful way to die is a complex yet vital topic that touches on medical, ethical, and spiritual dimensions. By understanding the biological aspects of death, the role of palliative care, and the various methods available, individuals and their families can make informed decisions about end-of-life care. It is crucial to approach this subject with sensitivity, respect, and a commitment to dignity and comfort.
We invite you to take action by sharing this article with others who may benefit from its insights. Consider discussing these topics with your loved ones and healthcare providers to ensure your preferences are understood and respected. Additionally, explore other resources and articles on our site to deepen your understanding of end-of-life care and related issues.